Abstract
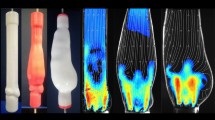
The abnormal growth of tissue, called pannus, is frequently found in patients who have an implanted prosthetic heart valve. Its growth is related to the valve dysfunction and disturbed blood flow in the aorta. We performed in vitro experiments to demonstrate the effects of pannus formation on hemodynamics and valvular function. The results showed that the opening angle of the heart valve changes depending on the size and shape of the pannus. The circular pannus decreased the maximum opening angle of the heart valve. Although the opening motion of the valve was not affected by the semi-circular pannus, one of the valve leaflets obstructed by the semi-circular pannus had a closing dysfunction during the cardiac cycle, implying aortic insufficiency and regurgitation in the patients with this type of pannus formation. The experimentally measured pressure gradient and velocity-based transvalvular pressure gradient estimation increased with the growth of the pannus, although a discrepancy between the two estimations was observed.
Similar content being viewed by others
References
J. B. Soumoulou, T. F. Cianciulli, A. Zappi, A. Cozzarin, M. C. Saccheri, J. A. Lax, R. Guidoin and Z. Zhang, Limitations of multimodality imaging in the diagnosis of pannus formation in prosthetic aortic valve and review of the literature, World J. Cardiol., 7 (2015) 224–229.
N. Piazza, S. Bleiziffer, G. Brockmann, R. Hendrick, M. A. Deutsch, A. Opitz, D. Mazzitelli, P. Tassani-Prell, C. Schreiber and R. Lange, Transcatheter aortic valve implantation for failing surgical aortic bioprosthetic valve: from concept to clinical application and evaluation (part 1), JACC Cardiovasc Interv., 4 (2011) 721–732.
M. Kondruweit, F. A. Flachskampf, M. Weyand, J. Schmidt, S. Achenbach and T. Strecker, Early failure of a mechanical bileaflet aortic valve prosthesis due to pannus: a rare complication, The Journal of Thoracic and Cardiovascular Surgery, 136 (2008) 213–214.
M. S. Chung, D. H. Yang, D. H. Kim, J. W. Kang and T. H. Lim, Subvalvular pannus formation causing aortic stenosis in patient with a normal prosthetic aortic valve: computed tomography finding, Eur. Heart J. Cardiovasc. Imaging, 16 (2015) 458.
R. Roudaut, K. Serri and S. Lafitte, Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations, Heart, 93 (2007) 137–142.
C. R. Bonnichsen and P. A. Pellikka, Prosthetic valve thrombus versus pannus, Circulation: Cardiovascular Imaging, 8 (12) (2015).
R. Roudaut, S. T. Lafitte, M.-F. Roudaut, C. Courtault, J.-M. Perron, C. Jaïs, X. Pillois, P. Coste and A. DeMaria, Fibrinolysis of mechanical prosthetic valve thrombosis: a single-center study of 127 cases, Journal of the American College of Cardiology, 41 (2003) 653–658.
G. Huang, H. V. Schaff, T. M. Sundt and S. H. Rahimtoola, Treatment of obstructive thrombosed prosthetic heart valve, Journal of the American College of Cardiology, 62 (2013) 1731–1736.
J. Barbetseas, S. F. Nagueh, C. Pitsavos, P. K. Toutouzas, M. A. Quiñones and W. A. Zoghbi, Differentiating thrombus from pannus formation in obstructed mechanical prosthetic valves: an evaluation of clinical, transthoracic and transesophageal echocardiography parameters, Journal of the American College of Cardiology, 32 (1998) 1410–1417.
S. Aoyagi, Doppler echocardiographic diagnosis of malfunction of a St. Jude Medical mitral valve, Artif. Organ. Today, 3 (1994) 299.
R. F. Carey and B. A. Herman, Limitations in the applicability of the simplified Bernoulli relation to aortic stenosis, Echocardiography, 11 (1994) 437–443.
A. Licata and W. H. Matthai Jr., Evaluating the etiology of mechanical valve obstruction: use of clinical parameters, fluoroscopy, and echocardiography, Catheter. Cardiovasc. Interv., 55 (2002) 495–500.
E. Konen, O. Goitein, M. S. Feinberg, Y. Eshet, E. Raanani, U. Rimon and E. Di-Segni, The role of ECG-gated MDCT in the evaluation of aortic and mitral mechanical valves: initial experience, AJR Am. J. Roentgenol., 191 (2008) 26–31.
H. Ha, H. J. Koo, H. K. Huh, G. B. Kim, J. Kweon, N. Kim, Y. H. Kim, J. W. Kang, T. H. Lim, J. K. Song, S. J. Lee and D. H. Yang, Effect of pannus formation on the prosthetic heart valve: in vitro demonstration using particle image velocimetry, PLoS One, 13 (2018) e0199792.
T. Yagi, W. Yang and M. Umezu, Effect of bileaflet valve orientation on the 3D flow dynamics in the sinus of valsalva, Journal of Biomechanical Science and Engineering, 6 (2011) 64–78.
J. M. Toole, M. R. Stroud, J. M. Kratz, A. J. Crumbley 3rd, S. M. Bradley, F. A. Crawford Jr. and J. S. Ikonomidis, Twenty-five year experience with the St. Jude Medical mechanical valve prosthesis, Ann. Thorac. Surg., 89 (2010) 1402–1409.
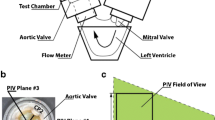
J.-W. Choi, J. H. Choe, S. Y. Jung, H. Park and H. Ha, Fabrication of affordable pulse duplication system for the in-vitro cardiovascular experiments based on gear pump and orifice flowmeter, Journal of Mechanical Science and Technology, 33 (2019) 3927–3932.
W. Thielicke and E. J. Stamhuis, PIVlab — towards user-friendly, affordable and accurate digital particle image velocimetry in MATLAB, Journal of Open Research Software, 2 (2014).
C. O. Lima, D. J. Sahn, L. M. Valdes-Cruz, S. Goldberg, J. V. Barron, H. D. Allen and E. Grenadier, Noninvasive prediction of transvalvular pressure gradient in patients with pulmonary stenosis by quantitative two-dimensional echocardiographic Doppler studies, Circulation, 67 (1983) 866–871.
H. J. Koo, H. Ha, J.-W. Kang, J. A. Kim, J.-K. Song, H. J. Kim, T.-H. Lim and D. H. Yang, Impact of pannus formation on hemodynamic dysfunction of prosthetic aortic valve: pannus extent and its relationship to prosthetic valve motion and degree of stenosis, Clinical Research in Cardiology, 107 (2018) 554–564.
K. Han, D. H. Yang, S. Y. Shin, N. Kim, J.-W. Kang, D.-H. Kim, J.-M. Song, D.-H. Kang, J.-K. Song and J. B. Kim, Subprosthetic pannus after aortic valve replacement surgery: cardiac CT findings and clinical features, Radiology, 276 (2015) 724–731.
H. Nygaard, P. K. Paulsen, J. M. Hasenkam, E. M. Pedersen and P. E. Rovsing, Turbulent stresses downstream of three mechanical aortic valve prostheses in human beings, The Journal of Thoracic and Cardiovascular Surgery, 107 (1994) 438–446.
P. D. Stein and H. N. Sabbah, Turbulent blood flow in the ascending aorta of humans with normal and diseased aortic valves, Circulation Research, 39 (1976) 58–65.
J. C. Cleveland, I. M. Lebenson and J. R. Dague, Early postoperative development of aortic regurgitation related to pannus ingrowth causing incomplete disc seating of a Björk-Shiley prosthesis, The Annals of Thoracic Surgery, 33 (1982) 496–498.
P. S. Mullenix, C. J. Parsa, G. B. Mackensen, J. G. Jollis, J. K. Harrison and G. C. Hughes, Pannus-related prosthetic valve dysfunction and life-threatening aortic regurgitation, The Journal of Heart Valve Disease, 17 (2008) 666–669.
A. K. Schaefer, M. Andreas, P. Werner, C. G. Sassi, T. Haberl, A. Kocher, G. Laufer and M. Russo, Excessive pannus overgrowth on the aortic side of trifecta valve causing severe regurgitation, The Annals of Thoracic Surgery, 108 (2019) e87–e89.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea, which is funded by the Ministry of Education (2018R1D1A1A0 2043249).
Author information
Authors and Affiliations
Corresponding author
Additional information
Hojin Ha received his B.S. at POSTECH, Korea, in 2009. He obtained his Ph.D. at POSTECH, Korea, in 2015. He is currently an Assistant Professor in the Department of Mechanical and Biomedical Engineering, Kangwon National University, Korea. His research interests are in the areas of experimental fluid dynamics.
Rights and permissions
About this article
Cite this article
Kang, J., Kim, D., Lee, Y. et al. Fluid-dynamic effect of pannus formation around the prosthetic heart valve: in vitro demonstration using a heart-mimic pulsatile pump and particle image velocimetry. J Mech Sci Technol 35, 209–220 (2021). https://doi.org/10.1007/s12206-020-1220-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12206-020-1220-2